Home » Posts tagged 'voice of the patient'
Tag Archives: voice of the patient
Improving Patient Satisfaction Via Lean Six Sigma
Lean Six Sigma in Healthcare Learn how The Juran Institute used Lean Six Sigma to help a medical telemetry unit in a medium-sized hospital, increase their HCAHPS percent ratings.
Problem Statement
A medical telemetry unit, in a medium-sized hospital, reported HCAHPS percent ratings below the competition for “Overall Unit Rating” and “Would You Recommend This Hospital.” The baseline scores of 9–10 responses on “Overall Unit Rating” were 56% and the percentage of “Definitely Yes” responses for “Would You Recommend This Hospital” was 61%.
Project Goals
The team defined the project goal to meet or exceed the highest percent ratings in the county for “Overall Unit Rating” and “Would you Recommend This Hospital” by:
- 0 – 20% improvement by November 2009
- 20 – 50% improvement by January 2010
- 50% improvement by March 2010
Project Team
The team was composed of representatives from the Telemetry Unit, Physical and Occupational Therapy, Pharmacy, Food and Nutrition Services, Respiratory, Care Coordination, Environmental Services, Transportation, Materials Management, Organizational Development, and Center for Nursing Practice.
Project Scope
The project scope was unsecured patient accounts. The beginning boundary for the project was the time a patient arrived in the E.D. The ending boundary was when the patient was discharged from the E.D. and financial responsibility was secured.
SIPOC Process
The team proceeded to develop a SIPOC (Supplier, Input, Process, Output, and Customer) on the “admission to discharge” patient process. This high-level process map is used to identify suppliers at the front end affecting the process, materials and inputs entering the process, materials and outputs exiting the process, and ultimately, customers impacted by the process.
Understanding the Needs of the Medical Telemetry Unit’s Audiences
The team conducted patient, family, and staff surveys and interviews to collect voice of the customer data on the patient’s experience. The team understood the importance of engaging the patient and family in the design of their care.
They acknowledged that it is not about the organization behind the services, rather it is about how the patient receives those services. In other words, it is all about the patients’ perception of their experience. The team took verbatim voice of the customer (VOC) data and translated it into themes and critical-to-quality requirements (CTQs). CTQs are defined as measureable customer needs and are considered by the team as solutions are designed and implemented.
Below are examples of the voice of the customer data from a patient’s perspective.
Several patients and family members commented that they have never been
asked before what is important to them and what the staff could do to provide the best experience. The team translated voice of the customer to key themes/issues and identified a critical to quality measure for affinity groups.

Understanding the Process
The team created a current state value stream map from the time the patient was admitted to the floor until discharge. Mapping proved to be challenging for the team due to the variation in care processes.
Understanding Non Value Added Work
The team analyzed the current state value stream map from the time the patient was admitted to the floor until discharge. The analysis helped the team identify non-value added work, bottlenecks, and issues impacting the patient experience.
Generating Solutions
Solutions were generated, prioritized and ranked by the Team. Five design teams were created: Patient Hospitality and Comfort, Discharge Preparation, Patient Education, Staff Education, and Noise Level. The project teams designed their solutions around key patient-centered design principles.
Shared Decision-Making
Patients vary widely regarding how much information they want and how much of a role they wish to play in making decisions. The Patient Discharge Team developed several robust strategies to encourage shared decision-making. With input from patients and families, the team created a patient communication board which serves two purposes: first, to provide information to the patient and family such as activity level and when the next pain medication is due, and second, to provide an opportunity for the patient to communicate with caregivers and physicians things that are important to them during their stay. It also helped to plan for discharge by recording the date and time of expected discharge. Patients and families are oriented to the board during the admission process (example board is shown below).
The team also designed patient discharge rounds every afternoon with the Care Coordinator, Unit Director, and Manager in order to identify patients for early discharge the next day. In addition, a discharge checklist was instituted.
Patient Education About Their Disease Process
The primary purpose of this education is to increase the patient’s understanding and responsibility for care. The Patient Education Team developed a Patient Guide on Congestive Heart Failure. The guide provides a roadmap for patients regarding what to expect each day during their hospital stay. The team also developed a list of questions for patients to ask upon admission and included them in the Patient Admission Guide.

Patient Engagement in the Design of Their Care
Patient and family needs were considered by the Patient Hospitality and Comfort Team. The team developed a tagline: “Going the extra mile to make our patient smile” and implemented the following solutions based on expressed needs:
- Waterless shampoo
- Hourly patient rounds to improve patient comfort and safety
- Scripting: addressing patients by name, sitting during conversations with patients and asking the patient upon leaving the room, “Is there anything else I can do for you before I leave? I have the time.” Also, telling the patient when you will return.
Staff Engagement in the Patient’s Care
The Staff Education Team developed a monthly newsletter to enhance communication amongst caregivers, management, and physicians. The newsletter discussed new clinical practices, changes to processes, educational offerings, and a story about a key contact. The staff also developed a Unit Performance Excellence Scorecard so that everyone understood what quality metrics were being monitored, how often, and the current status of performance. The language on the unit changed and staff began to link solutions to performance metrics.
Patient Centered Environment
The Noise Team was tasked to reduce the noise level on the unit and improve the cleanliness of the environment. The team implemented more frequent room checks, nursing and environmental manager morning rounds to identify areas that needed more personal attention, quiet hours from midnight to 5 AM, lowering ring tones on desk phones, and the use of Spectra Link® phones and OptiVox® to standardize patient handoffs.
Ensuring Long Term Solutions
The Control Phase provides the necessary methods and tools for an organization to hold the gains and continually improve the patient experience.
The team completed the necessary plans and transferred ownership of the plans to the Unit Director.
- Control plan: Provides roadmap of actions to hold the gains and continue improvement.
- Communications plan: Describes how and when information of process changes will be disseminated to staff and other key stakeholders throughout the organization.
- Training plan: Defines the training content, schedule, and outcomes for training staff on new process changes.
- New and revised policies and procedures: Documentation representing revised processes.
Results
Perseverance and commitment by the team to meet on a monthly basis following two rapid improvement events resulted in their exceeding all project goals. The team is likely to see even greater results in the future as they continue to listen to the voice of the customer and implement new solutions.

HCAHPS scores for “Would You Recommend” have shown a steady increase since September of 2009, improving nearly 35% in 5 months. The Standard HCAHPS Overall Average scores have shown an increasing trend over six months, culminating in a high score of 93.8%.
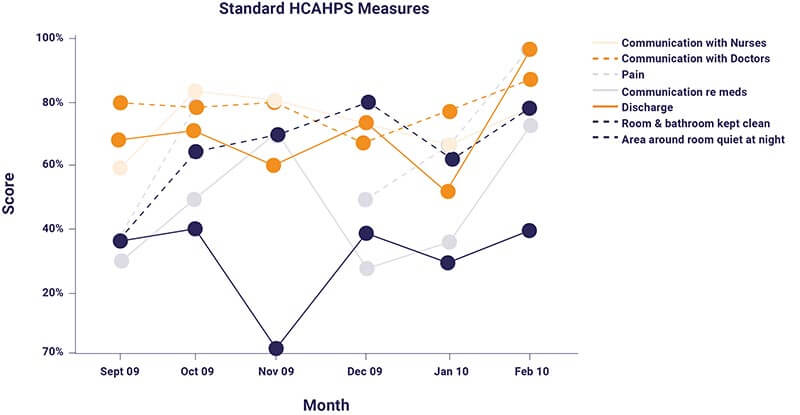
Upward trends for each of the HCAHPS measures are evident as of February 2010. Each measure has an improved score when compared with the initially recorded scores in September 2009.
I trust this article has provided you with insight and approaches that can help you pinpoint those drivers that most strongly influence a patient’s willingness to recommend a hospital. If you are interested in learning more about using these methods, contact us at: TPMG Global® – Improving HCAHPS Scores and The Patient Experience






